After dealing with the many annoying symptoms of endometriosis, and the long path to diagnosis many people with endometriosis come to learn that their fertility may be compromised. For many, this can be devastating news to receive whether you’re trying to conceive in the near future or want the option to try to become pregnant one day.
Upon receiving an endometriosis diagnosis, some of the first questions you might have been “what about my fertility?”, “Will I have trouble conceiving?’’ or “Am I at an increased risk of miscarriage or pregnancy complications?”. Often women are aware that their fertility will be impacted but deeper than that it is not commonly understood why this is.
Today we will be exploring some of the science behind why it may be more difficult to conceive with endometriosis. But first, let’s explore some of the statistics behind fertility and endometriosis.
Please note this blog post mentions topics surrounding fertility and miscarriage.
How common are fertility issues amongst those with endometriosis?
Up to 50% of endo warriors will have trouble falling pregnant, and up to 50% of people who do have struggles with fertility are diagnosed with endometriosis (Giudice & Kao, 2004). After all, infertility can be the only symptom some can experience of endometriosis.
From these numbers, it’s quite evident that endometriosis makes up a significant proportion of female factor infertility and sub-fertility. All hope is not lost though, this does not automatically mean that you cannot get pregnant with endometriosis. And you certainly shouldn’t rely on your diagnosis of endometriosis as contraception if you’re actively avoiding pregnancy! It just means that it MIGHT take longer to conceive, or you may need a bit more assistance from your medical or fertility team. And sadly, without actually trying to conceive, it’s impossible to know who may or may not become pregnant with ease. It is important to flag any concerns you have about your fertility, or preserving your fertility with your healthcare team.

So what are the top 5 potential reasons and explanation behind why it’s more difficult to conceive with endo?
1. Decreased egg quality
Inflammation is a characteristic component of endometriosis and is defined by a type of non-specific immune response. Research has shown that people with endometriosis are more likely to have higher levels of circulating oxidative stressors which are not only contributing to the pain and inflammation that you may be experiencing but may also contribute to the damage of the egg cells that reside within the ovaries (Nasiri et al., 2017).
Hang on, what’s all this oxidative stuff you’re talking about?
Reactive oxygen species (ROS) are types of unstable molecules that easily react with other molecules in a cell. Reactive oxygen species are produced from processes in the body, however, there is also a high percentage that comes from outside sources (e.g. smoking, alcohol, and pollutant exposure).
I think you can see where this is going right?
Simply put – increased levels of inflammation, (chronic or acute) and therefore reactive oxygen species, have the potential to damage the quality of your eggs. Luckily – this is one of the major things that can be improved significantly with nutrition and other lifestyle strategies, and in a relatively short space of time – about 3 months or so!
Want to learn more about Eating for Endometriosis? Join us for our LIVE masterclass on Thursday March 31st 2022 at 7pm AEDT for Endometriosis Awareness Month where we will be covering Anti-Inflammatory Eating for Endometriosis. Save your seat for this 60 minute jam-packed experience complete with eGuide, meal plan and Q&A time plus proceeds are being donated to the Pelvic Pain Foundation of Australia. Be quick! Save your seat today.
2. Issues with successful implantation
Similar to inflammation and oxidative stress having an impact on egg quality, inflammation in the pelvic region can make it difficult for ‘foreigners’ (i.e. an embryo) to make a comfortable home in the uterine lining. Recurrent implantation failure may be more common for those with untreated endometriosis (Zhong et al., 2021). Research has shown that those with endometriosis receive medical treatment for endometriosis that can improve fertility and pregnancy outcomes during IVF treatments, including improved rates of implantation (Zhong et al., 2021).
Learn more about what to eat for implantation here

3. Possible decreased ovarian reserve
Endometrioma, which is the presence of endometrial tissue on or in the ovary can damage the eggs. Ovarian reserve is decreased if you have endometrioma, and some research suggests there is a more rapid decline in AMH compared with those of the same age who do not have endometriosis (Hanege, Çekıç, & Ata, 2019). Unfortunately, the research also shows that there is a decrease in ovarian reserve post excision surgery of endometrioma (Hanege, Çekıç, & Ata, 2019) and this is likely due to the physical trauma surrounding the ovary and/or in some circumstances, where ovaries cannot be salvaged due to the damage caused by endometriosis, an ovary may be removed by a surgeon, obviously reducing egg quantity.
Whilst egg quantity is an important factor when it comes to available fertile years, it does not necessarily predict how easy or difficult it may be to conceive, so focusing on practical strategies around egg quality and maintaining ovarian reserve as best as possible is key.
4. Adhesions/scarring of fallopian tubes and ovaries
Endometriosis can cause adhesions on or in the ovaries and the fallopian tubes.
These can cause inflammation as they grow, and sometimes even bleed during periods. The body does its thing and responds to this inflammation, by causing more inflammation (great, isn’t it?) and forming scar tissue to attempt to ‘heal’ the endometriosis (Alimi et al., 2018).
This can make it difficult for eggs to be released effectively from the ovary, and to travel down the fallopian tube for fertilisation and then toward the uterus for implantation.
Large adhesions on the ovaries can also reduce blood supply to the area, and trap blood in the ovaries leading to cysts and damage (Alimi et al., 2018). The surgery itself is a risk factor for adhesions, given that there is trauma to the pelvic area, the goal of surgery is to have as few surgeries as possible with maximum time between surgeries being as symptom-free or close to that, as practical
It is vital you have a doctor or surgeon who is willing to answer all your questions and explain any procedure for your unique circumstances, and the effect it may have on your endometriosis progression and your future goals of expanding your family.

5. Comorbidity with other uterine structural abnormalities
Turns out, endometriosis may not be the only thing that may be impacting your fertility! People with endometriosis are more likely to also have endometrial polyps, which are non-cancerous growths of endometrial tissue in the inner wall of the uterus, as well as fibroids which are also non-cancerous growths made up of dense connective tissue that grows within the muscle wall. This risk is slightly increased for stage 2 – 4 endometriosis (Zheng et al., 2015). Endometrial polyps may be a cause for unexplained infertility for endometriosis. Removal of the polyp and appropriate medical management can increase the rate of pregnancy (Shen et al., 2011), as it logically reduces any structural feature which is getting in the way of a potential embryo implanting.
Overall, there are many ways that your fertility may be impacted with endometriosis. The most important feature of all of these contributors is that having a great health care team behind you can improve your chances of successful conception. Each factor can be mitigated or improved with the help of medical, or nutritional intervention. Working on your endometriosis management prior to conceiving can really be the best investment you can make for your current and future fertility health.

What does the research say about pregnancy outcomes and endometriosis?
Many of those with endometriosis who are thinking about pregnancy in the near or distant future, are not only worried about the potential delays to conception but also about the health of their pregnancy.
The findings surrounding pregnancy outcomes and endometriosis to date are quite mixed.
Some studies say that complications in pregnancy related to endometriosis are rare, and there is no major impact on pregnancy (Maggiore et al., 2016).
Whilst other studies show there is an increased risk of miscarriage, and ectopic pregnancy. Research has also shown an increased risk of complications during delivery such as preterm birth, placenta previa and excess bleeding (Saraswat et al., 2017). It is important to note that most people with endometriosis do have a normal, uncomplicated pregnancy and delivery.
Read more about how diet can impact pregnancy outcomes amongst those with endometriosis here

Need help with building an anti-inflammatory diet that suits your needs for endometriosis to support conception and throughout pregnancy? Check out our power-hour on-demand online Anti-Inflammatory Eating for Endometriosis masterclass, eGuide and meal plan designed for those with endometriosis by an expert endometriosis dietitian & nutritionist!
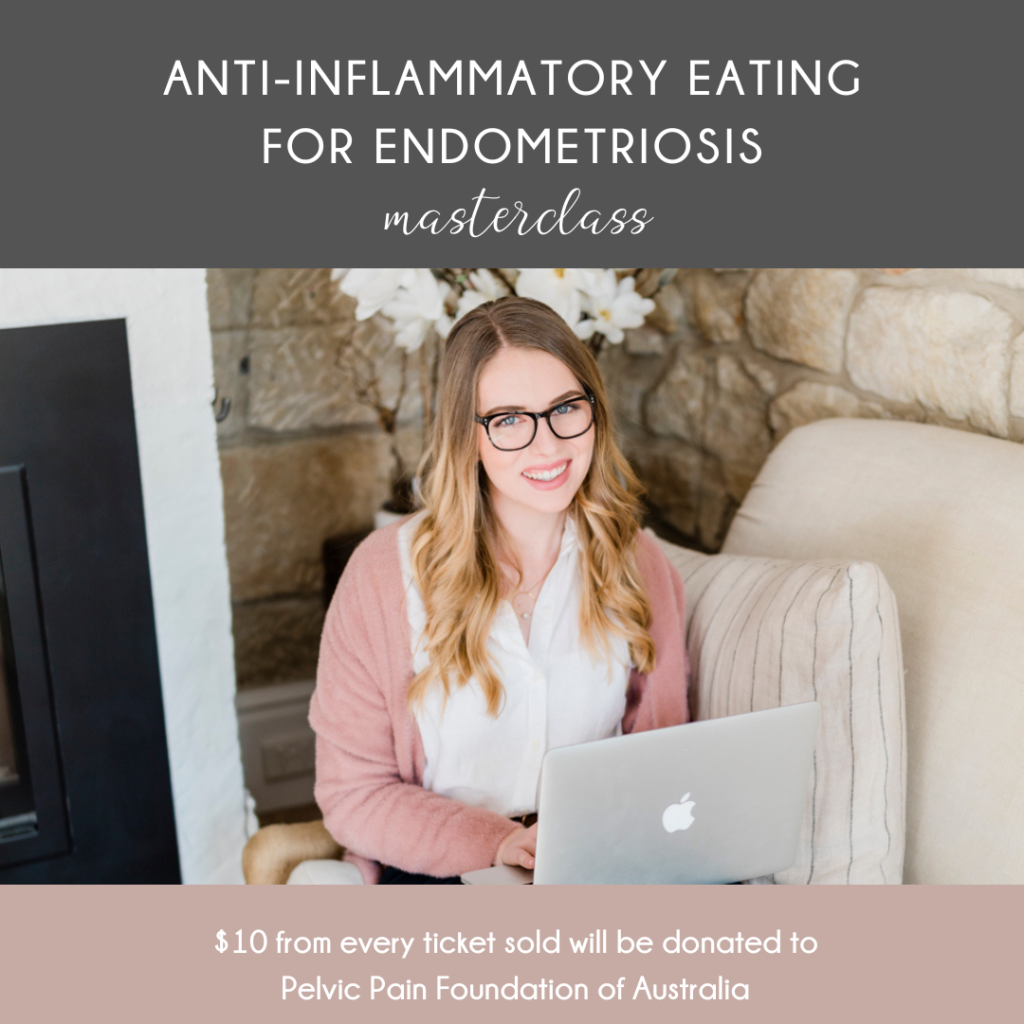
Available to start NOW for just $75 AUD (with $10 being donated to the Pelvic Pain Foundation of Australia). Can’t wait to see you there!